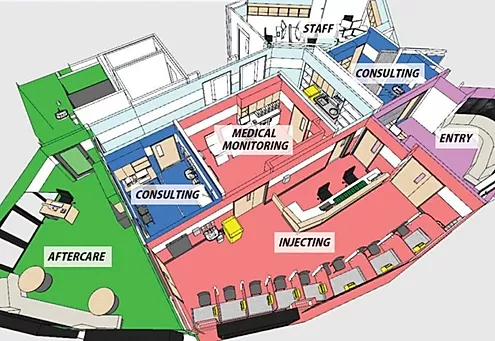
Overdose Prevention Centres (OPCs) are hygienic, safe spaces where people are able to take drugs safely under the supervision of trained staff. They have access to sterile equipment and staff can respond immediately to overdose.
In different jurisdictions and political environments OPCs are also sometimes called Supervised Drug Consumption Facilities (SDCFs), Supervised Injection Facilities (SIFs), Drug Consumption Rooms, or other variations.
OPCs also provide an opportunity for brief interventions and advice, or for people to be referred to drug treatment, mental health services, wound care, blood testing and other support.
There are currently approaching 200 OPCs in operation across the world in at least 18 countries including Canada, Germany, Switzerland, France, Portugal, Scotland, Ukraine, Norway, the Netherlands, Australia, Belgium, Spain, Denmark, Iceland, Mexico, Colombia, the US and Czechia.
In different jurisdictions and political environments OPCs are also sometimes called Supervised Drug Consumption Facilities (SDCFs), Supervised Injection Facilities (SIFs), Drug Consumption Rooms, or other variations.
OPCs prevent overdose deaths
OPCs reduce needle sharing that can lead to infections, including HIV and hepatitis C, as well as public injecting and discarded needles.
OPCs help increase numbers entering treatment and accessing other health and support services
OPCs are cost-effective reducing costs to health services and police.