Overdose Prevention Centres (OPCs) are hygienic, safe spaces where people are able to take drugs safely under the supervision of trained staff. They have access to sterile equipment and staff can respond immediately to overdose.
OPCs also provide an opportunity for brief interventions and advice, or for people to be referred to drug treatment, mental health services, wound care, blood testing and other support.
There are currently approaching 200 OPCs in operation across the world in at least 17 countries including Canada, Germany, Switzerland, France, Portugal, Ukraine, Norway, the Netherlands, Australia, Belgium, Spain, Denmark, Iceland, Mexico, Colombia, the US and Czechia.
OPCs prevent overdose deaths
OPCs reduce needle sharing that can lead to infections, including HIV and hepatitis C, as well as public injecting and discarded needles.
OPCs help increase numbers entering treatment
OPCs are cost-effective reducing costs to health services and police.
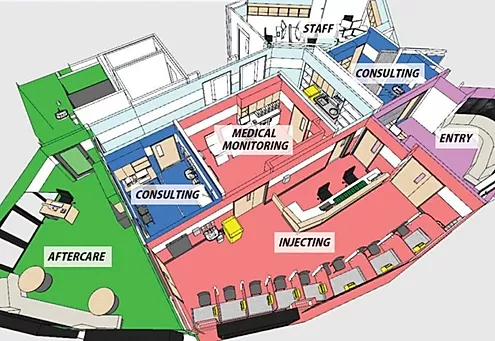
On entering the OPC, a new client's health status and drug use are briefly assessed. They then receive sterile equipment and have access to a clean booth where they can inject under the care of a nurse or other trained staff.
Clients then move to a recovery area for observation until safe to leave. Staff provide safer injecting advice, first aid, and overdose reversal treatment if needed. They may also offer referral to treatment and other services.
The best way to understand how an OPC works is to look inside.
You can also see how Canada's first OPC, Insite works, and one of Denmark's early mobile units
Injecting drug use happens everywhere. It happens inside homes, but also in the street. Too often the places where people take drugs are unhygienic, dangerous or isolated. Such places make dangerous infections more likely, and make it much harder to deal with overdose.
Until they are able to stop taking drugs, people who are dependent need safer spaces where they can inject. It can help save their lives, as well as helping reduce issues such as discarded needles.
Many local areas are exploring the possibility of opening an OPC. The Scottish Government has now overcome opposition from Westminster and will open a centre in Glasgow with NHS Scotland to help tackle record drug deaths and an HIV outbreak.
The UK Government announced it will not interfere with Glasgow's centre and the leader of the Labour Party, Keir Starmer, also said he would respect the wishes of the Scottish Parliament. This backing down creates an easier path for other places in England, Wales and Scotland to open one too.
OPCs are supported by many health bodies, police commissioners, NGOs and the Advisory Council on the Misuse of Drugs with recognition of their potential to reduce harm.
In Glasgow, a mobile OPC was first opened by Peter Krykant - acting ahead of any changes to the law. This 'guerrilla' facility changed the debate in Scotland and across the UK.
There is a large body of literature describing and evaluating Overdose Prevention Centres. Find some of the key studies here.
Canada has opened almost 150 supervised consumption sites. These pages explain why, and the steps to get permission to open one
This short video about the Dr Peter’s Hospice OPC has strong supportive quotes from the local residents association, housing, police, and business community. They have also produced Guidance on Community Consultation and Engagement for Implementation of OPCs.
Planning for a Supervised Injection facility Webinar on steps to open a OPC in the UK. Speakers include Prof Alex Stevens, Megan Jones (West Mids PCC Office), DCI Jason Kew, Niamh Eastwood (Release), Dr Saket Priyadarshi (Glasgow NHS), Rudi Fortson QC
- Overdue for a Change: Scaling Up Supervised Consumption Services in Canada
- Supervised Injection Services Toolkit Toronto Drug Strategy June 2013
- British Columbia: Guidance for setting up a DCR
- BC Supervised Consumption Services: Operational Guidance
- Registered Nurses Association of Ontario. Implementing Supervised Injection Services
Communities may have concerns about the opening of an OPC in their neighbourhood. It is key to consult, inform and educate everyone in advance. In some cases, OPCs have been delayed by opposition based on a misunderstanding of the likely outcomes.
When local residents and families affected by drugs are involved, however, support can be built.
For example:
- This short video about the Dr Peter’s Hospice OPC has strong supportive quotes from the local residents association, housing, police, and business community.
- In Melbourne, a group of residents and affected families called the Victoria Street Drug Solutions campaigned for an OPC to open in their area, which it did in 2018. Plans for a second one have now been announced.