24th March 2020
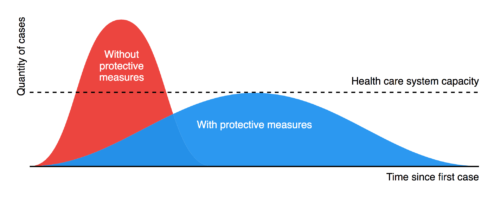
The COVID-19 crisis has now left an impact on every aspect of our lives. The recent, unprecedented, social distancing rules have been widely accepted on the basis that this is an issue of shared risk. For now, most of us are prepared to give up core liberties in order to protect vital services and ‘flatten the curve’.
At a time like this, it is easy to overlook the needs of the most marginalised in our communities. As we, rightly, look to protect the most vulnerable among our families – the old, and people with underlying conditions – we also need to remember those who have little or no social support at this time. The homeless, and people with alcohol or other drug problems, almost always fall to the bottom of the list when it comes to political action: which is partly why the swingeing cuts to services in recent years has been allowed to continue. At a time like this, the risk of marginalisation is further increased.
On compassionate grounds, we need to ensure services are not only retained but increased. However, this is also true if we want to protect the wider community. We understand that the priority for Government is to reduce, as far as is possible, the impact of COVID-19 on the community at large, and to ‘flatten the curve’ of infections to prevent the healthcare system from being overwhelmed. It is vital to remember, however, that any failure to support people who use drugs problematically will have very significant knock-on effects for the wider community. Loss of support in this area will have a disproportionately significant impact on healthcare capacity, as these communities are liable to be more vulnerable to both infection and the worst impacts of the virus.
Action in this area is vital for the wider effort to protect society as a whole. At a time when we are all learning to understand that personal and social risks are intimately connected, we must not forget that this extends to everyone in the community.
Working with Release, we submitted a response to the Treasury Committee’s call for evidence on the Government financial package for COVID-19. We focussed on the need to ramp up support for people with drug problems, for the reasons set out above. Our report contains fourteen recommendations. You can read the full submission here, and our recommendations are set out below.
- People who are dependent on drugs, including alcohol, must be categorised as one of the high-risk populations for COVID-19. Failure to protect the 320,000 people dependent on drugs, most with underlying health issues, will lead to vastly increased pressure on the NHS.
- The coronavirus is expected to lead to an unprecedented increase in demand for drug treatment services. Funding for this area should be increased dramatically to address the needs of some of the most marginalised and vulnerable in society, and reduce the numbers infected with COVID-19.
- Treatment providers will also have to implement prescription and other procedures that operate outside of existing guidelines to reduce social contact and protect the lives of staff and people who use drugs. This approach needs to be supported by Government and relevant agencies.
- The Mayor of London is moving towards securing hotel rooms across the capital for this population of people. Funding should be provided to other cities and towns to implement the same approach. This should include accommodation for those not ready or able to stop using drugs.
- We understand that there will be a national prescription delivery service for the vulnerable who are ‘shielded’. The delivery of controlled drugs, such as methadone and buprenorphine, must be included in medications that can be delivered.
- Systems must be put in place to ensure that there continues to be an adequate supply of harm reduction supplies, including sterile injecting equipment, that is flexible in the way it is dispensed to ensure social distancing rules are observed.
- Funding must be in place to ensure a significant supply of naloxone (an anti-overdose medication) is available for people who use opiates, particularly if fentanyl enters the market if the heroin supply is constrained.
- Funding should be made available to drug treatment providers to ensure they can fund innovative approaches, including peer outreach programmes, mobile services, and exploring the possibility of using existing and new premises to dispense equipment and medication, including OST (i.e. methadone or buprenorphine) and naloxone.
- All initial conditionality for claiming sickness benefits, including the limited capability for work/work-related activity (LCW/LCWRA) component of Universal Credit (UC), should be suspended for 12 months – this should also apply to work related benefits.
- All social security tribunals should be suspended, and appellants who are currently in receipt of reduced benefit payments as they await the outcome of their appeals, should be switched to full entitlement for 12 months.
- Suspension of eviction proceedings for tenants should be extended beyond the current 3 months, and should have an indefinite hold on place. This measure should also apply to those who are already subject to existing possession proceedings. Local authorities should be provided with additional funds for Discretionary Housing Payments to support those with a shortfall in rent.
- There should be a de-prioritisation in drug supply enforcement in order to protect people and to prevent more harmful substances entering the drugs market. Police forces should immediately end the stop and search, and arrest of people who use drugs to focus on more urgent issues related to COVID-19.
- It is imperative that, as other countries have done, prisoners are released where feasible and where there is no risk to society. Funding will be necessary to transition people back into the community, as well as ensuring wraparound services, in particular relating to those who have a history of drug dependency.
- Funding for mental health services is crucial, additional resources must be provided to allow for remote counselling services, including phone appointments, especially in light of the deleterious effect the crisis is having on people’s mental well-being.
James Nicholls, CEO at Transform Drug Policy Foundation
24/03/20